Photo: UNICEF Cambodia, Antione Raab
CHRONIC DISEASES: A GLOBAL PANDEMIC
Chronic diseases have risen to the top as the leading causes of death and disability worldwide. Once considered a problem for the elderly in developed nations has now become a global pandemic. In 2012, over 50% of adults in the U.S. had one or more chronic disease. By 2020, chronic diseases will account for 73% of all deaths across the globe. However, nearly 80% of these deaths will occur in developing countries. The inequitable distribution of resources and access to healthcare will ultimately result in the greatest harm to the most vulnerable populations.
Cambodia, like many other developing nations, is experiencing a rise in noncommunicable diseases (NCDs), pervasive and long-term ailments that include cancer, chronic respiratory disease, diabetes mellitus, and cardiovascular disease. There are various determinants that can contribute to the rising prevalence of NCDs, including genetics, lifestyle choices, and the environment. While negative behaviors can often be changed through targeted public health interventions, ultimately, the social and physical environments must also change in order to support individuals in making healthier choices.
From a macro perspective, the current health status of Cambodia’s population is greatly influenced by its economic state of development and health care infrastructure. Ranked as a low-income country by the World Bank, Cambodia has a Gini coefficient of 31.8 and a Gross National Income (GNI) of $2,890 per capita. 15 For the population of 14,865,000, inequity is high across socio-economic groups and noticeably different between rural and urban areas. This unequal distribution of wealth and resources inevitably impacts access to care. For instance, greater health care barriers are faced by 80% of the population, who populate rural and remote areas with minimal access to medical treatment facilities. Additionally, poverty is another barrier to care, as 45.9% of the population lives on less than $1.25 per day. 12 As a result, nearly half of Cambodia’s population struggles to obtain daily necessities and is unable to afford the high cost of medical care, which accounts for over 60% of total health expenditures. 12

Photo: Global Witness, Chean Chenda

Photo: Daily Mail.uk
It has also been speculated that the lack of access to health care has contributed to the country’s lower life expectancy at birth, which according to the World Health Organization (WHO) is 75 years for females and 70 years for males. 12 Furthermore, the crude birth rate is 25 live births per 1000 people, while the crude death rate is 6.70 deaths per 1000 people. 17 Additionally, the fertility rate is 2.9 births on average per woman over a lifetime. 11 All of these factors are contributing to the rising demand for health care to both meet the needs of the growing population and minimize preventable deaths. 11
The greatest suffering is experienced in rural communities, which lack access to available health care providers to adequately meet their needs. In 2008, there were only two physicians and eight nurses/midwives available for every 10,000 people living in rural areas. 17 Additionally, by 2011 there were only eight health facilities and 72 hospital beds available for every 100,000 people. 17 However, during the same year, there were 710 new nursing graduates and 134 new medical school graduates. 13 This illustrates that while the number of nurses entering the health care workforce was and is promising, the shortage of physicians and lack of available health care facilities still remains problematic.
In addition to a lack of medically trained providers, rural communities face numerous obstacles in accessing care. For one, quality is a major concern. A substantial part of the population, approximately 21%, receives care from the private non-medical sector, which is comprised mostly of traditional and religious healers. 13 This is concerning since most of these private facilities are not actively regulated, thus, making the quality of assurance questionable. Similarly, 49% of medical treatments occur through private facilities where quality assurance and regulation is minimal. 17 As a result, this negatively impacts the ability to prevent (via screening), treat, and manage NCDs for the most affected groups (e.g. low socio-economic status). This environmental barrier must change in order to provide greater access to health care nationwide.
While Cambodia has many environmental obstacles, there are also several opportunities that can be utilized to improve public health. For instance, the increasing rates of education can be a means to share knowledge and facilitate change. Currently, the primary school enrollment rate is at 98% and the total adult literacy rate is at 77.6%. 12 Education may serve as an outlet to inform the public on the negative consequences of poor behaviors (e.g. smoking) and how to alternatively make healthier choices.

Photo: UNDP
Another opportunity is to utilize the international aid coming into Cambodia. In 2010, contributions targeting health care reached $199 million.12 However, more than half of this aid went towards treating communicable diseases, such as HIV, TB and Malaria. A focus on infectious diseases has swept across the international community, non-governmental organizations (NGOs) and the Cambodian government. Multi-sectoral collaboration (including many of the 30 aid partners), has given rise to new policies, which focus monetary funds primarily on lowering infectious disease rates. The implications of such an agenda is that the prevention and treatment of many noncommunicable diseases may be overlooked.
In order to develop a broad and accessible healthcare system that benefits all people, a stronger emphasis needs to be placed on the prevention and treatment of NCDs. Based on current rates, chronic diseases will have the greatest impact on population health overtime. The result of this focus will inevitably be perceived in the near and far future. Ultimately, a greater percentage of the population will benefit from access to healthcare and an improved standard of living overall.

Photo: Buffalotours
The Rising Burden of NCDs
Studies show that chronic diseases are increasing in prevalence, while communicable, maternal, neonatal, and nutritional causes of disability-adjusted life years (DALYs) are declining. 18 DALYs represent the number of healthy years lost to due disability or premature death. According to the World Health Organization’s 2014 Noncommunicable Diseases Country Profile on Cambodia, NCDs caused 44,200 deaths accounting for 52% of all total deaths. 15 By comparison, communicable, maternal, perinatal and nutritional conditions only accounted for 31,450 deaths or 37% of total deaths. 15 This trend has been quantified by various studies, which provide evidentiary support for why more agency should be placed towards the prevention, treatment and management of NCDs.
The Global Burden of Diseases, Injuries, and Risk Factors Study compared changes in disease rates in Cambodia from 1990 to 2010. 18 This study determined the greatest burden by the absolute number of DALYs lost and then ranked each disease from 1 (best) to 15 (worst) according to the age standardized DALY rates. In 1990, the leading causes of DALYs lost were due to lower respiratory infections (rank: 8), followed by diarrheal diseases (rank: 3), and then malaria (rank: 8). In 2010, the leading cause of DALYs lost still remained to be lower respiratory infections but with a lower ranking of 4. However, the disease with the second greatest burden was now ischemic heart disease (rank: 13), followed by stroke (rank: 12). Overall, from 1990-2010 lower respiratory infections declined by 50% while ischemic heart disease increased by 75% and stroke increased by 55%. 18 Additionally, diarrheal disease, which was once the leading cause of burden, showed the greatest decrease in DALYs by 50%. 18 Similarly, other communicable diseases have had great reductions in DALYs, such as malaria (40%), meningitis (25%), and tuberculosis (10%). 18 In contrast, from 1990-2010, many NCDs have increased in disease burden, such as diabetes (110%), Cirrhosis (85%), COPD (25%), and other cardio and circulatory diseases (20%). 18 This shows that infectious diseases are declining while NCDs are rising in prevalence and severity.

Photo: Paula Bronstein, Getty Images
Since 2010, the prevalence of NCDs has continued to rise. In 2014, 7,400 people suffered from a stroke, while diabetes prevalence rose to 229,000. 14 The annual environmental burden for cardiovascular disease was calculated at 4 DALYs per 1000 capita. 14 In addition, cancer now affects 6,842 males and 8,374 females in Cambodia. 21 The most common cancers in males include liver (1,444 cases), lung (796 cases), and colorectal cancer (445 cases). 21 By comparison, the most common female cancers are of the cervix uteri (1,512 cases), breast (1,255 cases), and liver (820 cases). 21 According to the WHO, the annual burden of lung cancer is 0.3 DALYs per 1000 capita, while for all other cancers is 2.0 DALYs per 1000 capita. 14 Overall, the burden of cancer is high, which means that there is a large number of preventable deaths that are associated with unhealthy environments.
NCDs cause tremendous suffering, especially for individuals who go untreated. This is compounded with the fact that a majority of NCD deaths occur in individuals under 60 years old, with males accounting for 56.2% and females accounting for 34.8%. 20 This is highly problematic since most NCD deaths impact the working population, which reduces the labor force in Cambodia. The economic impact is high, as the productivity losses associated with absences, accidents and disability were found to be 400% greater than the cost of treatment.26 Ultimately, the economy would benefit from increased population treatment for NCDs. However, when families have to contend with the early death and/or disabilities of a household financial provider, the families are pushed into poverty due to the high cost of chronic treatment. Therefore, it is clear that more cost effective prevention and treatment options are needed.

Photo: MSAVLC

Photo: ICRC
Major Determinants and Risk Factors of NCDs
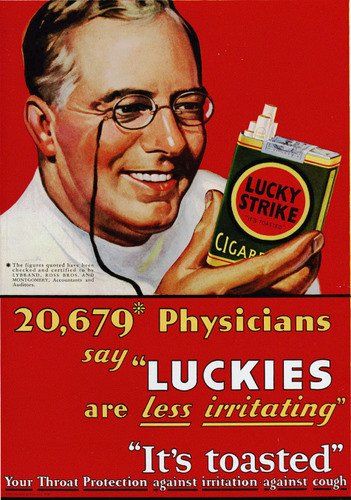
There are various underlying socio-economic, cultural, political, and environmental determinants of NCDs. For instance, globalization and urbanization have contributed to more sedentary lifestyles and the wide distribution of highly processed foods. Low-income households are large consumers of these high calorie, low nutrient items, due to their extensive availability and low costs. Similarly, current government policies in Cambodia make cigarettes affordable and widely available. For instance, at current rates, a pack of Marlboro cigarettes costs only $1.15, which is surprisingly less than the cost of a liter of Milk selling at $1.99. 25 The outcome is a physical environment that supports unhealthy behaviors, thus, enabling individuals to engage in common risk factors that are responsible for many chronic diseases.
This is evident in the high rates of modifiable risk factors such as unhealthy diets, physical inactivity, and tobacco use, as well as intermediate risk factors such as high blood pressure and obesity in the population. Currently, the prevalence of daily tobacco smoking among Cambodians is at 30%. 12 Also, 12.1% of the population is overweight, 11.2% are physically inactive, 2.1% are obese, and 27.6% have high blood pressure. 20 Furthermore, alcohol consumption is high at 5.5 liters per capita. 15 As such, it is no surprise that the leading risk factors that accounted for the greatest burden of disease in 2010 were dietary risks, household air pollution from solid fuels, and tobacco smoking, amongst others. 18
Of the total risk factors, dietary risks accounted for 9%, household air pollution accounted for 8.5% and smoking accounted for 7%. 18 These risk factors lead to cardiovascular and circulatory diseases, diabetes, cancer, diarrhea, lower respiratory infections, chronic respiratory diseases, and many other NCDs. Public health efforts should focus on educating and empowering the population on methods to minimize the risk of developing these high burdening diseases. For instance, behavior modification could target the four main modifiable risk factors, which include tobacco smoking, alcohol consumption, dietary risks, and physical inactivity. Engaging in these behaviors can drastically impact health. For example, smokers are 20 times more likely to develop lung cancer than those who have never smoked. 26 Similarly, inactivity and obesity resulting from poor diet increases the risk of death by at least 50%. 26 Thus, focusing policy and public health interventions on lowering these risks would dramatically aid in reducing NCDs.

Photo: Phnom Penh Post
Health Policy Suggestions
Prevention: reducing risk by targeting tobacco, alcohol, physical activity, and diet
In order to promote population health and well-being, education efforts should focus on the most wide spread and damaging habits. Scientific evidence has shown this to be smoking, alcohol consumption, physical inactivity, and unhealthy diets. 18 One method to change these behaviors is through policy change. For instance, public health interventions can be implemented in primary schools, which have high attendance rates and therefore, serve as prime locations to educate children on nutrition early on. Also, government subsidies for fruits and vegetables may help alleviate the financial barrier for those unable to afford fresh produce. Additionally, the Cambodian government could legislate to follow global agreements by supporting the commitments under the Framework Convention on Tobacco Control (FCTC). Furthermore, public smoking bans in certain areas (e.g. schools) and tighter advertising regulations may also help reduce current smoking rates. Overall, education should approach the four main risk factors with an aim to change social norms, all the while implementing policies that promote a healthier physical environment.

Photo: Khmer Times

Photo: Financial Times
Treatment: strengthening quality and access to primary health-care systems
Increasing quantity and quality of healthcare providers
A greater medical workforce is needed to keep up with population growth and the expanded coverage of care. One method to increase healthcare professionals, such as physicians and nurses, is by providing financial incentives (e.g. loan forgiveness) for students to pursue healthcare in Cambodia. However, before newly trained professionals enter the field, there needs to be a national standard for quality of care that is implemented and assured. In order to do so, the health workforce strategy must be revised, and training (both pre-service and in-service) must be strengthened. 12 Also, capacity building and knowledge sharing is needed in order to effectively spread information on standard treatment protocols and quality accreditation. This must occur across various health care groups, including the private sector and universities.
Increasing access to care – expanding coverage and reducing costs
One reason NCDs are negatively impacting Cambodia’s population is due to the lack of access to affordable quality care for screening, treatment, and disease management. However, the government has been making changes towards improving access. The Cambodian Government recently implemented the second Health Strategic Plan 2008-2015 (HSP2). Focus has now moved towards implementing the National Strategic Development Plan (NSDP) 2014-2018, which aims to improve population health and access to resources in a sustainable fashion. 12 One positive outcome is the expansion of Health Equity Funds (HEFs), which now cover 80% of the poorest people in the country and helps reduce the financial obstacles to receiving care. However, 20% of the poorest population still lacks access and the financial resources to obtaining quality healthcare. Therefore, this underserved population should be targeted through outreach services and facility based coverage. Strengthening and coordinating the resources of NGOs to assist in supporting the WHO’s Cooperative Strategic Agenda (2008-2015) may help achieve full coverage. 12 This would also support the development of a national social health protection policy and financing mechanisms that target the poor.
In addition, low-cost medications should be provided to high-risk patients (e.g. hypertensive) or those requiring long-term treatment due to chronic disease (e.g. cancer). With advancing technologies, cost effective strategies for NCD prevention and treatment are becoming more common. Optimism is high, as new strategies are estimated to prevent 80% of diabetes and global heart disease in the future. 26 For instance, high blood pressure can be effectively managed with medication at a low cost of only a few cents per day. 26
Furthermore, with expanded coverage, screenings for disease must also increase. This is vital, since many NCDs are not curable, and most have a slow onset and long duration. Thus, early detection combined with treatment and management will provide the greatest benefit for patients. This has occurred in many high-income countries which have had increased rates of survival due to cancer treatments combined with early detection and screening. 26 For instance, the 50-year relative survival rate for all cancers diagnosed in the US from 1975-1977 was 49% compared to 68% from 2004-2010, reflecting advances in treatment and early diagnosis. 24
Overall, a serious problem faces Cambodia. On the one hand, policy makers must consider how to manage the growing element of NCDs and how to reduce the negative physical, financial, and national burden that they have on the population. On the other hand, decision makers must utilize the countries current resources of international aid and upcoming policy reform in order to emphasize education and implement broad-based healthcare availability. Ultimately, in order to reduce the impact of NCDs in the future and improve the health of Cambodia’s population, policy efforts should focus on expanding healthcare coverage, reducing treatment costs, and both increasing and improving screening, treatment, and disease management.

Photo: UNICEF Cambodia
IF YOU ENJOYED THIS POST, PLEASE LIKE, SHARE & COMMENT BELOW
REFERENCES
- Cambodia: Demographic and Health Survey. National Institute of Statistics. Directorate General for Health, Ministry of Health, Cambodia. 2010. Web. Received from: http://dhsprogram.com/pubs/pdf/FR249/FR249.pdf
- Recent Fertility and Family Planning Trends in Cambodia. Department of Planning and Health Information, Ministry of Health, Reproductive Health Association of Cambodia, PRB. 2003. Web. Received from: http://www.prb.org/Publications/Articles/2003/RecentFertilityandFamilyPlanningTrendsinCambodia.aspx
- Data: Cambodia. The World Bank Group. 2015. Web. Received from: http://data.worldbank.org/country/cambodia
- Cambodia Falls Short of Early Childhood Nutrition Goals. Department of Planning and Health Information, Ministry of Health, Reproductive Health Association of Cambodia, PRB. 2003. Web. Received from: http://www.prb.org/Publications/Articles/2003/CambodiaFallsShortofEarlyChildhoodNutritionGoals.aspx
- Maternal Mortality a Leading Cause of Death in Cambodia. Department of Planning and Health Information, Ministry of Health, Reproductive Health Association of Cambodia, PRB. 2003. Web. Received from: http://www.prb.org/Publications/Articles/2003/MaternalMortalityaLeadingCauseofDeathinCambodia.aspx
- Degan, Guy. Lack of adequate sanitation triggers child health concerns in Cambodia. UNICEF. 7 May 2008. Web. Received from: http://www.unicef.org/infobycountry/cambodia_39558.html
- Shepherd-Johnson, Denise. Nutrition campaign helps make Cambodia’s children strong, health and clever. UNICEF. 24 April 2013. Web. Received from: http://www.unicef.org/infobycountry/cambodia_68872.html
- Shepherd-Johnson, Denise. In Cambodia, a push to bring healthcare to remote areas. UNICEF. September 2012. Web. Received from: http://www.unicef.org/infobycountry/cambodia_66038.html
- Cambodia- Poverty Reduction Strategy Paper and Joint Assessment. The World Bank Group. 2003. Web. Received from: http://documents.worldbank.org/curated/en/2003/01/2122042/capovertyreductionstrategypaperprspjointassessment
- Cambodia. The World Bank Group. 2015. Web. Received from: http://search.worldbank.org/all?qterm=cambodia&title=&filetype=
- 11. Cambodia: WHO Statistical Profile. World Health Association. 2012. Web. Received from: http://www.who.int/gho/countries/khm.pdf?ua=1
- Cambodia Country Cooperation Strategy: at a glance. World Health Organization. May 2014. Web. Received from: http://www.who.int/countryfocus/cooperation_strategy/ccsbrief_khm_en.pdf?ua=1
- Cambodia Population Statistics. World Health Organization. 2013. Web. Received from: http://www.who.int/gho/countries/khm.pdf?ua=1
- Cambodia Country Profile of Environmental Burden of Disease. World Health Organization. Public Health and the Environment, Geneva. 2009. Web. Received from: http://www.who.int/quantifying_ehimpacts/national/countryprofile/cambodia.pdf?ua=1
- Noncommunicable Diseases (NCD) Country Profiles, 2014. World Health Organization. 2014. Web. Received from: http://www.who.int/nmh/countries/khm_en.pdf?ua=1
- WHO Global Database on Vitamin A Deficiency. World Health Organization. 2007. Web. Received from: http://www.who.int/vmnis/vitamina/en/
- Western Pacific Health Databank, 2012-2013, Cambodia. World Health Organization. 2013. Web. Received from: http://www.wpro.who.int/countries/khm/4_khm_2012_final.pdf
- Global Burden of Disease Profile: Cambodia. Institute for Health Metrics and Evaluation. 2301 Fifth Ave., Suite 600, Seattle, WA. 2010. Web. Received from: http://www.healthdata.org/sites/default/files/files/country_profiles/GBD/ihme_gbd_country_report_cambodia.pdf
- Cause-Specific Mortality and Morbidity. World Health Organization. World Health Statistics 2009. Web. Received from: http://www.who.int/whosis/whostat/EN_WHS09_Table2.pdf
- Cambodia NCD Country Profiles, 2011. World Health Organization. 2011. Web. Received from: http://www.who.int/nmh/countries/khm_en.pdf?ua=1
- Cambodia. International Agency for Research on Cancer. World Health Organization. 2012. Web. Received from: http://gicr.iarc.fr/public/docs/20120906-WorldCancerFactSheet.pdf
- Tackling NCDIs in Cambodia: an opportunity for inter- and intra-sectoral synergies. Health, Nutrition, and Population Knowledge Brief. World Bank. 2014. Web. Received from: http://documents.worldbank.org/curated/en/2014/11/23070441/tackling-ncdis-cambodia-opportunity-inter-intra-sectoral-synergies
- Prevalence of Non-Communicable Disease Risk Factors in Cambodia. STEPS Survey, Country Report. Ministry of Health, Cambodia. 2010. Web. Received from: http://www.who.int/chp/steps/2010_STEPS_Report_Cambodia.pdf
- Cancer Facts & Figures 2015. American Cancer Society. 2015. Web. Received from: http://www.cancer.org/acs/groups/content/@editorial/documents/document/acspc-044552.pdf
- Cost of Living in Cambodia. NUMBEO. 2015. Web. Received from: http://www.numbeo.com/cost-of-living/country_result.jsp?country=Cambodia
- Wipfli, Heather. “Busting the Myths of NCDs.” University of Southern California. Lecture. 3 Feb. 2015.
- Cambodia. Water Aid. 2015. Web. Received from: http://www.wateraid.org/where-we-work/page/cambodia.
- Cover photo: http://timeoutvietnam.vn/Files/uploads/20151124/images/nhung-dieu-co-ban-can-biet-truoc-khi-du-lich-campuchia-3.jpg
APPENDICES
Table 1. Demographic and economic indicators for Cambodia
| Indicator |
Data |
Latest year |
Source |
| Total population |
15,205,539
14,865,000 |
2013
2014 |
11
15
|
| Crude death rate (per 1000) |
6.70 |
2004 |
17 |
| Crude birth rate (per 1000) |
25 |
2004 |
17 |
| Life expectancy at birth (yrs) |
72 (Both Sexes)
75 (Female)
70 (Male)
|
2012 |
12 |
| Total fertility rate |
2.9 per woman |
2013 |
11 |
| Total adult literacy (%) |
77.6% |
2008 |
12 |
| School Enrollment rate |
98% net, primary |
2012 |
3 |
| Ranked low, middle or high income? |
Low-income |
2012 |
3 |
| GNI per capita ($) |
$2,890 |
2013 |
13 |
| Gini coefficient |
31.8 |
2011 |
3 |
| Population living below $1.25/day (%) |
45.9% |
2010 |
12 |
|
Major imports
|
Refined Petroleum (10%)
Light Rubberized Knitted Fabric (10%)
Other Synthetic Fabrics (3.6%)
Raw Sugar (2.1%)
Gold (2%)
|
2014 |
3 |
|
Major exports
|
Postage Stamps (14%)
Knit Sweaters (12%)
Knit Women’s Suits (7.7%)
Non-Knit Women’s Suits (5.5%)
Non-Knit Men’s Suits (5.3%)
|
2014 |
3 |
| % deaths due to infectious disease |
20.16% |
2011 |
8 |
| % deaths due to NCDs |
52% |
2014 |
15 |
| Top 3 diseases (in terms of deaths): 1. Ischemic heart disease (10.1%), 2. TB (9.6%), 3. Stroke (8.7%) |
8.5
8.2
7.4
(Thousands) |
2012 |
11 |
| Top 3 diseases (in terms of DALYs lost): 1. Lower respiratory infections, 2. Ischemic heart disease, 3. Stroke |
6,600 (Age standardized DALYs 1-15: 4)
8,500 (Age standardized DALYs 1-15: 13)
7,400 (Age standardized DALYs 1-15: 12)
|
2012, Age stand. DALYs: 2010 |
18
11
|
| DALYs lost (%) |
N/A |
|
|
|
Top 3 causes of DALYs lost: 1. Maternal, neonatal, nutritional, 2. Other NCDs (non-malignant neoplasms; endocrine, blood and immune disorders; sense organ, digestive, genitourinary and skin diseases; oral conditions; and congenital anomalies), 3. Cardiovascular diseases and diabetes
Risk Factors accounting for most disease burden: 1. Dietary Risks, 2. Household Air Pollution, 3. Smoking
|
~ 820,000
~ 610,000
~ 600,000
9% DALYs
8.5% DALYs
7% DALYs |
2012
2010 |
11, 18
|
Table 2. Environmental situation for Cambodia
| Indicator |
Data |
Latest year |
Source |
| Environmental Health |
| Environmental Burden of Disease (%) |
Deaths: 25% of total burden |
2004 |
14 |
| Top 3 greatest contributors to environmental burden of disease (DALYs): 1. Diarrhea, 2. Respiratory Infections, 3. Unintentional injuries (other than road traffic) |
27
18
5.9
(DALYS/1000 capita) per year
|
2004 |
14 |
| Deaths due to Indoor Air Exposure (Deaths/year) |
6,600 deaths/year |
2004 |
14 |
| Deaths due to Outdoor Air Exposure (Deaths/year) |
300 deaths/year |
2004 |
14 |
| Global Climate Change Threat |
N/A |
|
|
| Water and Sanitation |
| Water Situation (scarcity) |
33% people lack access to safe water |
2008 |
27 |
| Population using improved water and sanitation (%) |
Sanitation:
22% (Rural)
76% (Urban)
Overall: 67%
Water:
61% (Rural)
90% (Urban)
|
2011 |
12 |
| Burden of Disease from Diarrheal Disease |
27 DALYs/1000 capita (per year) 10,000 children die/year |
2004
2014
|
14
27
|
Table 3. Maternal, child and nutritional health situation for Cambodia
| Indicator |
Data |
Latest year |
Source |
| Maternal health |
| Antenatal coverage, at least once (%) |
89% |
2010 |
1 |
| Antenatal coverage, at least four times (%) |
59% |
2010 |
1 |
| Skilled attendant at birth (%) |
71% |
2010 |
12 |
| Contraceptive prevalence (%) |
51% |
2007 |
11 |
| Maternal mortality ratio |
250/100,000 live births
170/100,000 live births |
2010
2013 |
12 |
| Child health |
| Annual number of under-five deaths |
40/1000 (38/1000 live births ) * 388,880 births = 14,777.44 deaths |
2012
2013
|
12
11
|
| Infant mortality rate |
45/1000 live births |
2010 |
17 |
| Child mortality rate |
Prob. of dying before age 15: M: 20%, F: 16% |
2012 |
11 |
| Neonatal mortality as proportion of all under-five mortality |
(18/1000 live births) * (38/1000 live births) = 0.47368 deaths (6,999.77 deaths/year)
18/1000 live births |
2012
2013 |
12
|
| Nutrition |
| Percent of babies born with low birth weight |
8.2% |
2012/13 |
17 |
| Children exclusively breastfed < 6 months (%) |
73.5% |
2012/13 |
17 |
| Children still breastfeeding 20-23 months (%) |
3.51% |
2010 |
1 |
| Children moderately or severely underweight (%) |
< 5 yrs old: 28% |
2012/13 |
17 |
| Children moderately or severely wasted (%) |
11% |
2010 |
1 |
| Children moderately or severely stunted (%) |
39.5% (under 5 years old: 40%) |
2012/ 2013
2014
|
17
12
|
| Vitamin A supplementation full coverage (%) |
71% |
2010 |
1 |
| Households consuming iodized salt (%) |
84% |
2010 |
1 |
| Children 1-year-old receiving measles immunization (%) |
90% |
2007 |
11 |
Table 4. Noncommunicable Disease situation in Cambodia
| Indicator |
Data |
Latest year |
Source |
| Major Diseases |
| Total # of NCD deaths |
44,200 |
2014 |
15 |
| % of NCD deaths to people under 60 yrs. |
Males: 56.2% Females: 34.8% |
2008 |
20 |
| Stroke |
7,400 Age Standardized Death rate: 101.49/100,000 ppl |
2014
2011
|
15
|
| COPD |
1.1 DALYs/1000 capita per year |
2004 |
14 |
| Diabetes prevalence |
229,000 |
2014 |
22 |
| Cancer Deaths & Cases |
Deaths: 13% = 11,050
Cases:
M: 6842
F: 8374
|
2014
2012
|
15
21 |
| Top 3 cancers (males) 1.Liver, 2. Lung, 3. Colorectal |
1444 cases
796 cases
445 cases
|
2012 |
21 |
| Top 3 cancers (females) 1. Cervix, 2. Breast,3. Liver |
1512 cases
1255 cases
820 cases
|
2012 |
21 |
| Risk Factors |
| Current Daily Tobacco Smoking prevalence (%) overall, males, females |
30%
42%
3%
|
2014
2011 |
12
15 |
|
Physical inactivity overall, males, females
|
11.20%
11.40%
11.10%
|
2008 |
17 |
| Alcohol consumption per capita |
5.5 liters |
2010 |
15 |
| Overweight (%) overall, males, females |
12.1%
10.8%
13.2%
|
2008 |
20 |
|
Obesity (%) overall, males, females
|
2.1%
1.5%
2.7%
|
2008 |
20 |